 BBC
BBC
Five times Prof Kevin Fong broke down in tears in a nondescript hearing room in West London, while giving evidence to the Covid inquiry.
The 53-year-old has the kind of CV that makes you pay attention: a consultant anaesthetist in London who also works for the air ambulance service and specialises in space medicine.
In 2020, as Covid spread around the world, he was seconded to NHS England and sent out to the worst hit areas to support other medics.
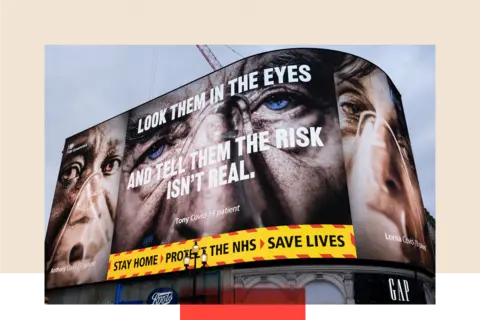
We’ve long been told that hospitals were struggling to cope during the pandemic. In January 2021, then prime minister Boris Johnson warned the NHS was “under unprecedented pressure”.
But now many hours of testimony to the Covid inquiry this autumn is offering our clearest understanding yet of what was really going on at the height of the pandemic.
The inquiry restarts its live hearings this week with evidence from doctors and patient groups. Health ministers and senior NHS managers are also expected to appear before the end of the year.
I was at the inquiry the day Prof Fong calmly talked through more than 40 visits he led to intensive care units, his voice cracking at times.
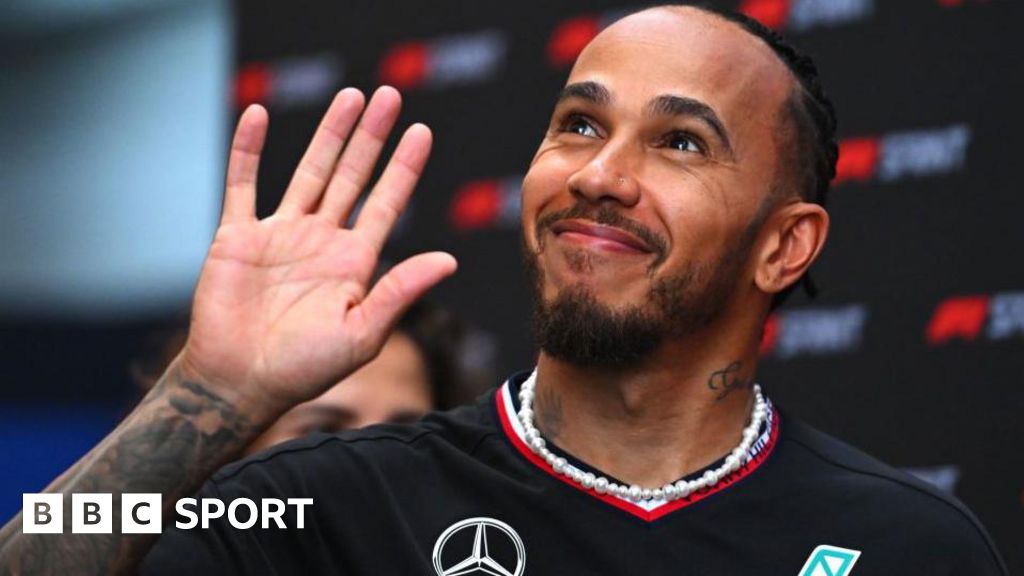
Prof Kevin Fong, a consultant anaesthetist, gave evidence to the Covid inquiry.
What Prof Fong discovered at the hospitals he visited was something he said could not be found in the official NHS data or the main evening news bulletins at the time.
“It really was like nothing else I’ve ever seen,” he said.
“These people were used to seeing death but not on that scale, and not like that.”
In late 2020, for example, he was sent to a midsize district hospital somewhere in England that was “bursting at the seams”.
This was just as the second wave of Covid was hitting its peak. England was days away from its third national lockdown. The first vaccines were being rolled out but not yet in large numbers.
In that hospital, he found the intensive care unit, the overflow areas and the respiratory wards all full with Covid patients.
The previous night someone had died in an ambulance outside waiting to be admitted. The same thing had happened that morning.
The staff were “in total bits”. Some of the nurses were wearing adult nappies or using patient commodes because there wasn’t time for toilet breaks.
One told him: “It was overwhelming, the things we would normally do to help people didn’t work. It was too much.”
That night, Prof Fong and his team helped to transfer 17 critically ill patients to other NHS sites – an emergency measure unheard of outside the pandemic.
“It is the closest I have ever seen a hospital to being in a state of operational collapse,” he said.
“It was just a scene from hell.”

 Getty Images
Getty Images
During the pandemic, hospitals cancelled much of their usual planned work
The full story
In the pandemic we heard reports of swamped hospitals in danger of being overwhelmed though to what extent was never fully clear.
On the face of it bed occupancy in England – that’s the total number of hospital beds taken up by all patients – did not hit more than 90% in January 2021, the peak of the largest Covid wave.
That’s above the 85% level considered safe but not any higher than a typical winter outside the pandemic.
That doesn’t tell the full story. At that point hospitals had cancelled all their usual planned work – from hip replacements to hernia repairs. Strict Covid rules meant the public were told to stay at home and protect the NHS. The numbers coming in through A&E in England fell by almost 40% compared to the previous year, to 1.3 million in January 2021.
That was why, when anti-lockdown protestors sneaked into hospitals to film, they found deserted corridors and rows of empty seats.
The pressure though was often being felt elsewhere – on the main wards and in intensive care units (ICUs), where thousands of the sickest Covid patients needed help to breathe on ventilators.
“At our peak we ran out of physical bed spaces and had to resort to putting two patients into one space,” one ICU nurse at a different hospital told Prof Fong.
“Patients were dying daily, bad news was being broken over the phone or via an iPad."
Later research by the Intensive Care Society found that in January 2021, 6,099 ICU beds were filled across the UK, well above the pre-Covid capacity of 3,848.
This huge spike in demand, equivalent to building another 141 entire intensive care units, was being driven by the length of time Covid patients needed treatment.
On average they would spend 16 days in ICU, normally on a ventilator, compared with just four to seven days for a patient admitted for another reason.
Surge capacity
As a result, hospitals had to rush to convert operating theatres, side rooms or other wards into makeshift intensive care units. NHS trusts often ended up juggling shortages of equipment, medicines and oxygen.
But while it might have been possible to cram in more beds, finding the extra skilled workers to staff them was far more difficult.
Prof Charlotte Summers, who led the intensive care team at Addenbrooke’s hospital in Cambridge, said: “We can’t just magic up specialist care staff because it takes a good couple of years, at least, for minimum critical care speciality training.”
“What we had, we had, and we had to stretch further and further.”
As a result staffing ratios were pushed to the limit in Covid, something she said politicians, the media and the public didn’t fully understand at the time.
Outside of a pandemic, specialist critical care nurses would be responsible for just a single patient. In Covid they were looking after four, five or even six – often all on a ventilator.
“Staff didn’t have time to process or accept the losses,” the lead ICU matron at one large teaching hospital told Prof Fong.
“As soon as one patient had passed away they had to get the bed cleared and ready for the next patient."
Others in intensive care and Covid wards – from doctors to pharmacists to dietitians – saw their workloads stretched well beyond normal safe levels.
This was the main reason why temporary Nightingale hospitals, built in the first Covid wave at a cost of more than £500m, only ever treated a handful of patients. It was possible to build the critical care infrastructure almost overnight, but quite another thing to find trained medics to work in them.
To help plug these staff shortages in ICU, volunteers were frequently brought in from other parts of the hospital, often with no experience of intensive care medicine or of dealing with that level of trauma and death.
“They were being exposed to things which they wouldn't necessarily be [exposed to] in their normal jobs, people deteriorating and dying in front of them, the emotional distress of that,” said Dr Ganesh Suntharalingam, an ICU doctor and former president of the Intensive Care Society.
Another hospital doctor said he felt some junior members of staff were “thrown in at the deep end” with little training and no choice about where they were sent.
The inquiry heard that all this “inevitably” had an impact on some of the sickest patients.
At no point did the NHS have to impose a formal ‘national triage’, where someone was refused treatment because they could not get a hospital bed.
But using that as measure of health system collapse may be too simplistic anyway.
Prof Summers said it would be mistake to think of “catastrophic failure” as a switch that goes “from everything being okay to everything not being okay the next second.”
“It is in the dilution of a million and one tiny little things, particularly in intensive care.”
She said when the system becomes so overstretched it feels like “we are failing our patients” and not providing the care “that we would want for our own families”.
New research suggests those hospital units under the greatest pressure also saw the highest mortality rates for both Covid and non-Covid cases.
Difficult decisions were having to be made about which of the sickest patients to move up to intensive care.
Those Covid patients who needed CPAP, a form of pressurised oxygen support, rather than a ventilator, often had to be cared for in general wards instead, where staff may have been less used to the technology.
One anonymous ICU doctor in Wales said: “We didn't have enough space to ‘give people a go' who had a very remote chance of getting better. If we had had more capacity, we might have been in a position to try."
The inquiry was also told that at least one NHS trust was under so much pressure it implemented a blanket “do-not-resuscitate order” at the height of the pandemic. If a patient went into cardiac arrest or stopped breathing, it would mean they should not be given chest compressions or defibrillation to try to save their life.
In normal times, that difficult decision should only be made after an individual clinical assessment, and a discussion with the patient or their family.
But Prof Jonathan Wyllie, ex-president of the Resuscitation Council, said he knew of one unnamed trust that put in place a blanket order based instead on age, condition and disability.
Groups representing bereaved families said they were horrified, adding it was “irrefutable evidence the NHS was overwhelmed”.

 Getty Images
Getty Images
There are almost 130,000 job vacancies in the NHS across the UK
Air ambulances
At times, the impact on intensive care was so great that some units had to undergo “rapid depressurisation” with dozens of patients transferred out, sometimes over long distances, to other hospitals.
Before the pandemic, from December 2019 to February 2020, only 68 of these capacity transfers had taken place in England. Between December 2020 and February 2021, 2,152 were needed, either by road or air ambulance.
Often it was the most stable patients in smaller district hospitals who would be selected for transfer as – bluntly – they were the most likely to survive in a moving vehicle for several hours.
“But what that meant for the smaller units is that they were left with a cohort of patients who were most likely to die,” said Prof Fong.
“Those units would experience mortality rates in excess of 70% in some cases.”
In normal times between 15% and 20% of ICU patients die in hospital, according to the Faculty of Intensive Care Medicine.
Prof Charlotte Summers gave evidence to the Covid inquiry.
Very human
Through the pandemic the NHS did continue to operate and, on a national basis, patients who really needed hospital treatment were not turned away.
But Prof Charlotte Summers, in her evidence, said staff are still “carrying the scars” of that time.
“You cannot see what we’ve seen, hear what we’ve heard, and do what we’ve had to do and be untouched by it,” she said.
“You cannot and be human. And we are very much human.”
Health services in all four UK nations started the pandemic with the number of beds in ICU and staffing levels well below average compared to other rich countries.
Five years on and there are still almost 130,000 job vacancies in the NHS across the UK. Sickness rates among the 1.5 million NHS employees in England are running well above pre-pandemic levels, with days lost to stress, anxiety and mental illness rising from 371,000 in May 2019 to 562,000 in May 2024.
All this comes as the health service struggles to recover from Covid with waiting lists for surgery and other planned treatments still hovering near record levels.
“We coped, but only just,” said Prof Summers and Dr Suntharalingam in their evidence to the inquiry.
“We would have failed if the pandemic had doubled for even one more week, or if a higher proportion of the NHS workforce had fallen sick.
“It is crucial to understand how very close we came to a catastrophic failure of the healthcare system.”
With the inquiry ongoing none of the agencies are currently commenting.
Additional reporting and research by Yaya Egwaikhide
Top photo credit: Getty
BBC InDepth is the new home on the website and app for the best analysis and expertise from our top journalists. Under a distinctive new brand, we’ll bring you fresh perspectives that challenge assumptions, and deep reporting on the biggest issues to help you make sense of a complex world. And we’ll be showcasing thought-provoking content from across BBC Sounds and iPlayer too. We’re starting small but thinking big, and we want to know what you think - you can send us your feedback by clicking on the button below.

 3 weeks ago
9
3 weeks ago
9